Poor circulation in the feet occurs when blood flow to the lower extremities is reduced, making it harder for oxygen and nutrients to reach the tissues. People may notice coldness, numbness, tingling, cramping, or skin that appears pale or discolored. Common causes include diabetes, peripheral artery disease, smoking, high blood pressure, and prolonged sitting or standing. Aging can also affect circulation, especially when combined with reduced activity levels or underlying medical conditions. Improving circulation often involves consistent movement throughout the day. Walking, ankle rotations, and gentle stretching help activate the muscles that support blood flow. Elevating the feet when resting, maintaining healthy hydration, and wearing shoes that do not restrict the forefoot or ankle can also be beneficial. Addressing chronic conditions and avoiding tobacco play an important role in long-term improvement. If foot circulation problems persist, it is suggested that you see a podiatrist for a proper diagnosis and appropriate treatment.
Poor circulation is a serious condition and needs immediate medical attention. If you have any concerns with poor circulation in your feet contact one of our podiatrists of Westside Podiatry Center, LLP. Our doctors will treat your foot and ankle needs.
Poor Circulation in the Feet
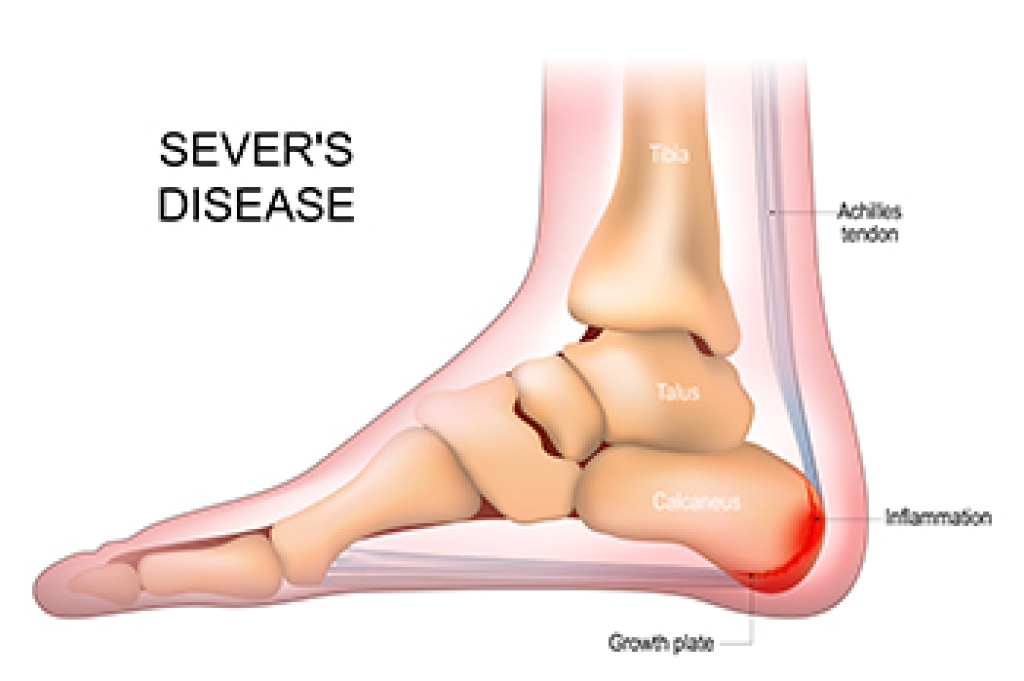
Poor blood circulation in the feet and legs is can be caused by peripheral artery disease (PAD), which is the result of a buildup of plaque in the arteries.
Plaque buildup or atherosclerosis results from excess calcium and cholesterol in the bloodstream. This can restrict the amount of blood which can flow through the arteries. Poor blood circulation in the feet and legs are sometimes caused by inflammation in the blood vessels, known as vasculitis.
Causes
Lack of oxygen and oxygen from poor blood circulation restricts muscle growth and development. It can also cause:
- Muscle pain, stiffness, or weakness
- Numbness or cramping in the legs
- Skin discoloration
- Slower nail & hair growth
- Erectile dysfunction
Those who have diabetes or smoke are at greatest risk for poor circulation, as are those who are over 50. If you have poor circulation in the feet and legs it may be caused by PAD and is important to make changes to your lifestyle in order to reduce risk of getting a heart attack or stroke. Exercise and maintaining a healthy lifestyle will dramatically improve conditions.
As always, see a podiatrist as he or she will assist in finding a regimen that suits you. A podiatrist can also prescribe you any needed medication.
If you have any questions, please feel free to contact one of our offices located in Liverpool, Camillus, Skaneateles, Oswego, and Cicero, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.